The clinical trial is aiming to understand how psilocybin alters brain function in order to improve treatment options for mental illness.
Led by the University of Minnesota Medical School (UoM), the study is also aiming to identify how long brain changes last in a bid to aid therapists in identifying a therapeutic window of opportunity for psychotherapy interventions.
Investigating the visual effects of psilocybin will illuminate general principles by which psilocybin might act on other circuits in the brain, including cognition, emotion and therapeutic outcomes, potentially yielding new scientific insights on the relationship between psilocybin and mental health.
The study is enrolling 46 carefully vetted participants with good physical health and experience taking psilocybin, but who do not have a current or previously-diagnosed major mental illness or substance use disorder.
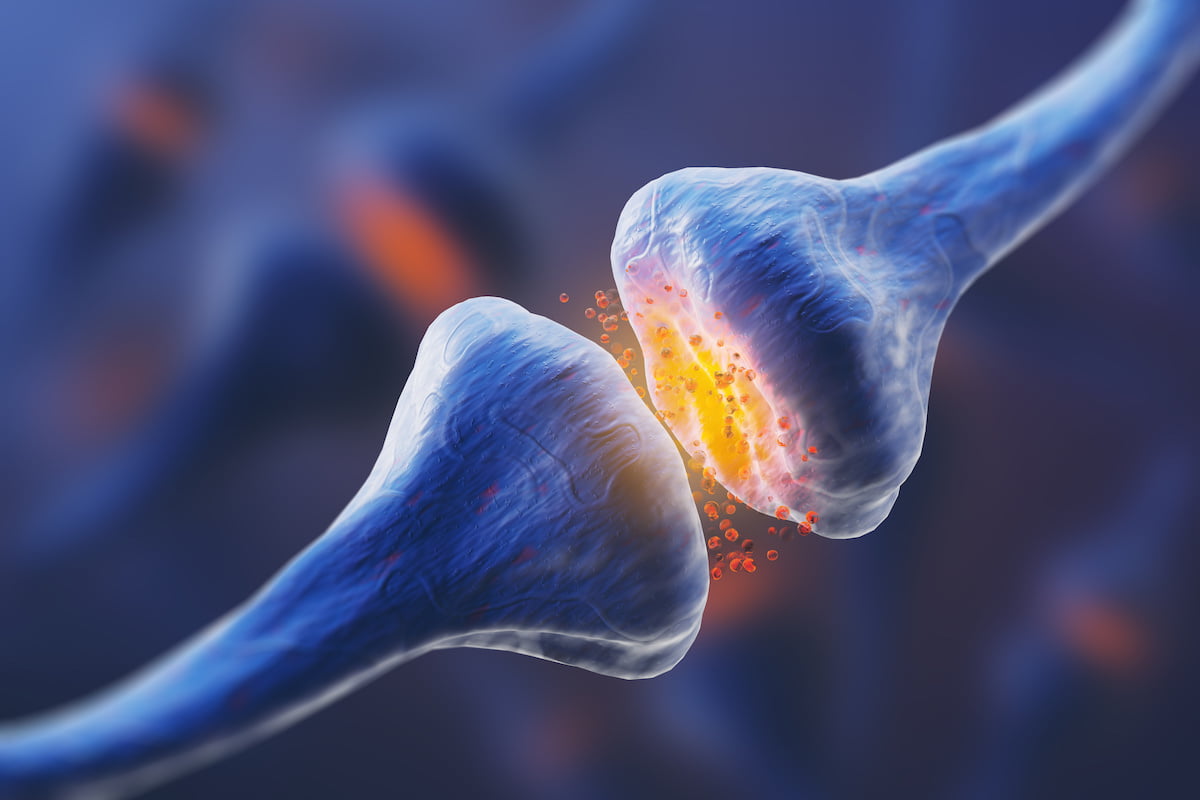
Lead investigator, Jessica Nielson, PhD, assistant professor in the Department of Psychiatry and Behavioral Sciences and core faculty at the University’s Institute for Health Informatics, commented: “One arm of the study, which is being led by predoctoral researcher Link Swanson, looks at visual perception and how it is affected by psilocybin. Another arm of the study is looking at the time-course of brain changes produced by psilocybin, using diffusion tensor imaging (DTI), a type of MRI scan that can visualise dendritic spines, which until now, has only been shown in animal models.
“The point is to enrol people who are comfortable with psilocybin and are able to navigate their own mind very well because they will be asked to do visual performance tasks while in an altered state of consciousness.”
Study participants will undergo a series of baseline tests to measure blood and brain biomarkers of neuroplasticity prior to taking psilocybin – including blood draws and MRI and EEG scans. They will then undergo one dosing session with psilocybin and one with a placebo (niacin).
Nielson continued: “It’s a triple-blind study, so neither the participants, researchers nor the statistician will know which compound participants get first, and we will monitor them the entirety of their session. During their session, they will be asked to wear an EEG and perform visual perception tasks on a computer.
“After that day, they come back three more times — the next day, three to four days after, and seven days after — for MRI scans. About a week after that, after the brain has had a ‘washout’ period, they will return for their second dosing session, where they will be given whatever study compound they didn’t have during their first session.”
An independent statistician will analyse all of the results, which Nielson hopes will provide new information about the mechanisms of how exactly psilocybin changes the brain and when.
“And, if we can figure out the time-course of this therapeutic window of opportunity, it also gives therapists a more informed protocol for how long they have after a dosing session to do integrative psychotherapy — exactly how long they have to harness the brain’s neuroplasticity to get that deeply-ingrained, pathological behaviour or belief changed.”
Nielson is seeking additional funding to grow her research team and maintain the pace of enrolment for the study, which is expected to have peer-reviewed results available by 2024. Tax-deductible donations to this study can be made to the PATH Fund through the University of Minnesota Foundation.

 Opinion2 years ago
Opinion2 years ago
 Insight3 years ago
Insight3 years ago
 Medicinal2 years ago
Medicinal2 years ago
 Research2 years ago
Research2 years ago
 Medicinal2 years ago
Medicinal2 years ago
 Markets & Industry1 year ago
Markets & Industry1 year ago
 News3 years ago
News3 years ago
 Medicinal2 years ago
Medicinal2 years ago
















