A new narrative review of systematic evidence has been published by leading researchers at Drug Science to get the facts on the adverse effects of classic psychedelics.
Classic psychedelics fall into the lowest risk category for drugs, the review findings show. This means they are non-toxic to the human body and have a very low dependence rate.
Published by non-profit organisation Drug Science in the Journal of Psychopharmacology, the paper highlights that policy has yet to catch up with the science – attributed largely to misinformation.
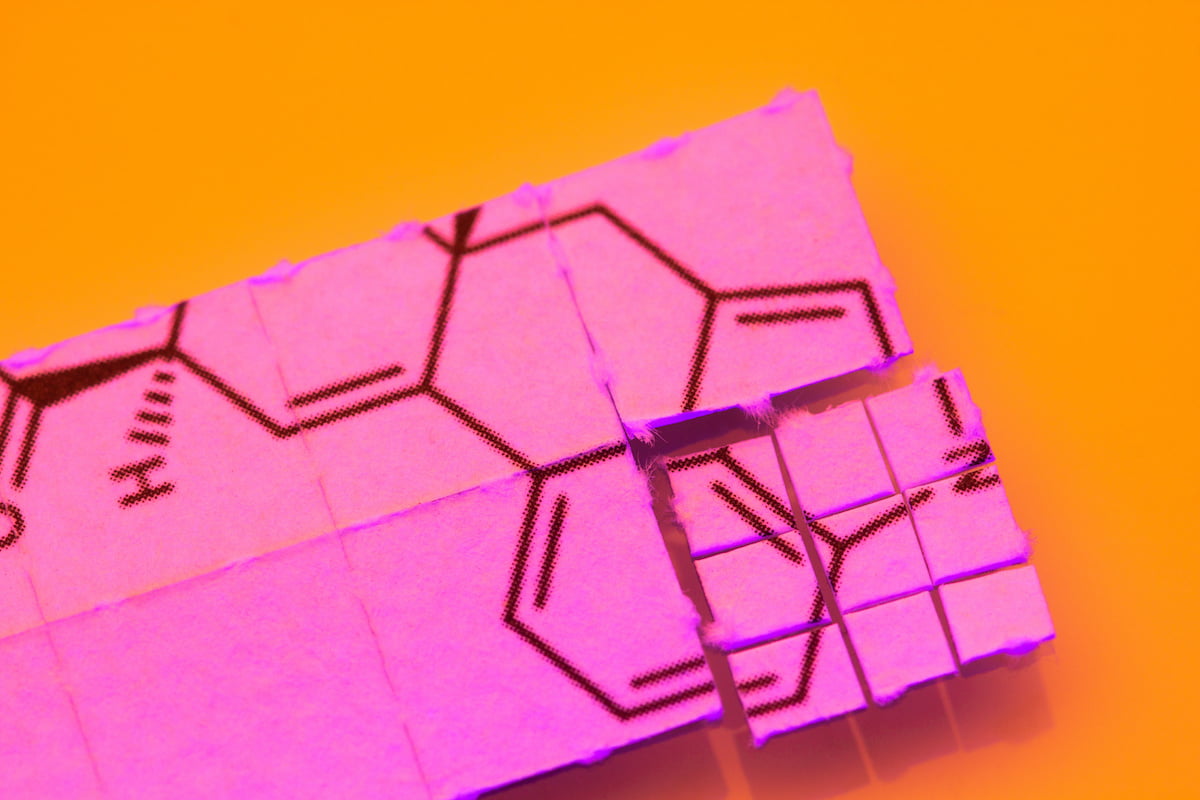
The authors focus on classic psychedelic compounds – serotonergic psychedelics such as psilocybin, DMT, ayahuasca, mescaline and LSD.
Authors include Dr Katrin Anne Schlag of Imperial College London and King’s College London, Jacob Aday of Central Michigan University and the University of California, Davis, Iram Salam, Professor Jo Neil of the University of Manchester, UK and Professor David Nutt of Imperial College London.
An unwarranted reputation
Decades of anecdotes have given psychedelic substances a reputation for being dangerous. Sensationalist reports of people losing their minds, getting hallucinogenic flashbacks or jumping off buildings have contributed to negative public attitudes towards these compounds.
In recent years, despite costly regulatory barriers, scientists at institutes such as Imperial College London, Harvard University, Johns Hopkins and many more, have been able to look more closely at them – revealing strong therapeutic potential in the areas of mental health and addiction.
Speaking to Psychedelic Health, paper co-author Dr Anne Katrin Schlag, head of research Drug Science, department of brain science, Imperial College London, and department of geography, King’s College London, commented: “Psychedelics previously received quite a bad reputation within the media and within the public domain, unreservedly so.
“One concern that people tend to have is that they are addictive and you can become dependent on them. Their scheduling as Class A together with heroin and cocaine would suggest this, but this is not based on scientific evidence.
“However, with the recent research, especially the past decade, and media reports of people who have actually have been helped and healed by various types of psychedelics, it seems there is now a move towards a more favourable attitude towards these substances From the public, as well as politicians, doctors and potential prescribers who are looking at the research in-depth.
“In our review, we are presenting the scientific evidence of various harms and look in detail at which of these are supported by the current science, and which are merely based on previous myths and negative perceptions.
“These substances are not new, and they have been studied before.”
The counterculture movement in the 60s saw an explosion of cultural liberation and experimentation with fashion, music and drugs. Prominent figures including Ken Kesey, Allen Ginsberg, Timothy Leary, Richard Alpert and Aldous Huxley – as well as popular musicians such as Jim Morrison, Jimi Hendrix, Gerry Garcia and Janis Joplin – were all experimenting with LSD.
Frequent reports of their use led to the perception that the compounds had a high dependence rate. In 1971 Nixon declared the worldwide “war on drugs”, labeling drug abuse as “America’s public enemy number one”. The same year, psychedelics were scheduled in the highest category of the UN Convention on Psychotropic Substances.
By this time there was a large body of research into the use of LSD in humans, reporting largely positive effects but with significant shortcomings. The paper highlights: “The emergence of 1960s counterculture, led to a media frenzy and sensationalised representations of these substances, contributing to the halt of promising scientific research and national and international [under the 1971 UN Conventions] bans on LSD”.
Schlag commented: “Before Nixon declared the war on drugs there was quite a lot of promising research with psychedelics such as LSD, but due to their increasingly bad reputation within the counterculture movement, and sometimes not sufficiently high ethical research standards, this research came to a standstill.
Find out what the decriminalisation of psychotropic substance cultivation means for the Right to Science
“We found some of this earlier research, in addition to the current research, and looked at it in detail, to actually find that there were few medical risks reported – and there were thousands of patients during that period of time as well.
“All drugs or substances – legal or illegal – have risks but we do know that if you look at the medical risks, such as toxicology, neurotoxicity, hypertension, cardiovascular disease, classic psychedelics consistently rank very low in comparison to other substances.
“When there are issues, these tend to be resolved very quickly – within the session usually – and are transient.
“The potential for addiction is very low as well. Some of these substances have now been shown to be anti-addictive and could actually help people with addiction very substantially.”
Psychedelics are undeserving of their current scheduling
Timothy Leary, Richard Alpert and Ralph Metzner’s work, The Psychedelic Experience, based largely on the Tibetan Book of the Dead, emphasises “set and setting” as fundamental to the positive psychedelic experience.
The new paper echoes this importance for clinical outcomes when using these compounds: “Looking at differences between clinical vs non-clinical uses and users, we stress that whilst these categories are blurred and use and users might be overlapping between categories, notable differences can be discerned in users’ set and setting, as well as the pre- and aftercare experienced – both areas where above adverse effects are potentially exacerbated.”
Schlag et al highlight some of the common challenging experiences induced by classic psychedelics are “bad trips”, but these are quite rare and “are often found to be extremely cathartic”.
“When we are looking at medical uses of psychedelics in a clinical environment – in a safe setting, under supervision, where the patient is fully supported before, during, and after the session with integration by a fully trained psychiatrist or therapist – then these adverse effects are extremely rare,” said Schlag.
“What has also been shown globally now with the multi-criteria decision analysis work that Drug Science is doing, which was first published in The Lancet in 2010, they consistently rank very low.
“Especially for magic mushrooms – classic psychedelics are undeserving of their current scheduling. We have done multi-criteria analysis regularly to analyse the harms of drugs, and not just the individual health harms and physiological harms, but also the societal harms and the harms to others.”
More research is needed
The authors conclude that it is vital that clinicians and therapists keep to the highest safety and ethical standards and that balanced media reporting is also key in “avoiding future controversies, so that much needed research can continue”.
Schlag said: “We need more research to be funded and to reschedule psychedelics so that the research can actually happen easier and become less costly. I think we have only just started to see their potential, but this has to be done extremely carefully in a regulated environment.
“People reading about it and taking a psychedelic to heal their PTSD, for example, could potentially be very damaging if they are in an unsafe environment because these are very strong drugs – they need to be administered and taken in a safe set and setting.
“However, that is not to say that there’s no room for non-clinical applications, because a lot of these plant medicines have been used for millennia, very successfully, within various cultures.
“I think we are really very much at a crossroads – psychedelics will be able to help a lot of people but we have to be cautious, because a lot of these people are also very ill and need to be treated correctly within the medical – or otherwise safe – environment.
“At the moment, the main issue is that’s not really possible because our Western society does not allow access to these medicines.”
To read the full paper please visit journals.sagepub.com/doi/full/10.1177/02698811211069100.
[activecampaign form=52]

 Opinion2 years ago
Opinion2 years ago
 Insight3 years ago
Insight3 years ago
 Medicinal2 years ago
Medicinal2 years ago
 Research2 years ago
Research2 years ago
 Markets & Industry1 year ago
Markets & Industry1 year ago
 Medicinal2 years ago
Medicinal2 years ago
 News3 years ago
News3 years ago
 Research2 years ago
Research2 years ago