Co-founder and CEO Anthony Tennyson spoke to Psychedelic Health about Awakn’s mission to transform mental health and addiction care through psychedelics.
Biotechnology company Awakn Life Sciences has established the first-ever network of psychedelic-assisted therapy clinics in the UK and is developing the next generation of psychedelic therapeutics.
Its two-pronged approach of clinic provisions and drug development aims to provide transformative healthcare – combining drugs and therapies to better treat addiction and other mental health conditions such as anxiety, depression, PTSD and eating disorders.
Co-founded by Tennyson and world-leading psychedelic scientist and psychiatrist Dr Ben Sessa, the company has a robust team of experts in the field.
The team includes leading addiction scientist and global authority on psychedelics, Professor David Nutt; expert in neuroscience drug discovery, Dr Shaun McNulty; expert in ketamine-assisted psychotherapy for addiction, Professor Celia Morgan; and leading psychologist, Dr Laurie Higbed. Awakn is also working with Steve Page as an independent non-executive director, who has helped to build the largest network of mental healthcare hospitals and clinics in the UK.
CEO Anthony Tennyson, commented: “Addiction is substance addictions like alcohol and tobacco, prescription drugs, behaviour addictions like gambling, and also sexual behaviour and binge eating disorders. These are massive problems that are poorly treated. We have the ability to do a much better job than the incumbent industry – that is why we decided to focus on addiction.”
In the last year Awakn has acquired a number of assets, including exclusive rights to the world’s only Phase IIb clinical trial looking at ketamine-assisted psychotherapy for treating Alcohol Use Disorder (AUD), carried out by professor Celia Morgan, and the world’s only Phase IIa clinical trial looking at MDMA-assisted psychotherapy, also for the treatment of AUD.
“The core purpose of the company is to democratise psychedelics for the better treatment of addiction,” said Tennyson. “We are developing therapeutic package therapies and drugs to be used together. We are working with MDMA and ketamine in the near term to develop the therapy, but we are also developing our own drugs and therapies together into a single package in due course.
“Historically, companies have tried to treat addiction in two ways – with drugs or with talk therapy. With drugs, there tend to be three approaches. Trying to switch off individual receptor sites to stop the binding of the active ingredient and therefore negating the effects of those drugs. In our opinion, that is not a long-term solution. Another approach is to switch off other binding sites that create a craving, which may be may or may not be effective – once you stop taking those drugs and the craving comes right back.
“The other approach is swapping out one drug for another – swapping heroin for methadone, for example. It is not very effective. And talk therapy is not always effective for people.
“There is a massive societal problem. 20 per cent of the planet is affected by substance addiction or have a substance addiction. Gambling disorder affects up to 6 per cent of the population on the planet – that is up to 400 million people. Compulsive sexual behaviour, which includes pornography addiction, affect 5 per cent – up to 350 million people.
“So, we are coming to treating addiction in a revolutionary way. We are targeting the brain circuits rather than individual receptors – targeting a multi-receptor approach. There are essentially three levels to your brain, lower, mid and upper. Upper is your cognitive function, mid is the salience attribution – the importance upon which your brain or your personality applies to certain things – and the lower level is memory formation and reward.
“What happens in a normal brain, is that the cognitive part of the brain has control over the whole system and the connections between the whole system and the cognitive part are strongest. In an addicted brain, the cognitive part actually shrinks and the reward attribution part of the brain grows.
“We are using drugs to provide temporary disruption between the connections of those circuit levels. That provides temporary relief, but, in the space that disruption provides, we bring in proprietary psychotherapy to enable people to understand why they have a predisposition to consumption of addictive substances. That gives us the ability to work across both substance and behavioural addictions.”
Awakn’s ketamine programme and its overall research strategy have been set by Professor Nutt, and its data from Morgan’s ketamine-assisted psychotherapy trial will be published in the American Journal of Psychiatry, later this year.
“When published it will indicate that ketamine is quite effective at treating alcohol use disorder in combination psychotherapy. So, we are the only company in the world delivering evidence-backed ketamine-assisted psychotherapy for Alcohol Use Disorder [AUD]. We are also going to be licensing that into the North American markets. We are in discussions to see how we can bring that forward into a Phase III trial so that we can execute on our purpose, and could potentially have ketamine on-label in the UK for the treatment of AUD.
“We have also initiated a mechanistic study in conjunction with the University of Exeter to assess ketamine in the context of gambling addiction. We believe memory plays quite an important part in the dynamic of gambling addiction, and ketamine is quite effective at disrupting memories.
“So, we are trying to see how ketamine affects memory, recall and reward mechanisms in the brain for people who have a problem with gambling. If that is effective, and if there is a positive correlation, we will then look to bring that forward into later-stage research and follow the same path as with AUD.
“For MDMA, David, Ben and Laurie ran the Phase IIa trial that was published in February of this year in the Journal of Psychopharmacology. Typically speaking, there is a 75 per cent relapse rate with AUD. The team had between a 30 and 20 per cent relapse rate with the six and nine-month observation. It is a small safety and tolerability trial, but that is a strong paradigm shift in results. We are working to bring that research forward from Phase IIa to Phase IIb and to develop the clinical trial protocol.
“We have submitted that to The Medicines and Healthcare products Regulatory Agency (MHRA) for scientific advice. We have received our scientific advice. We are updating the protocol and intend to submit that for clinical trial approval this calendar year.”
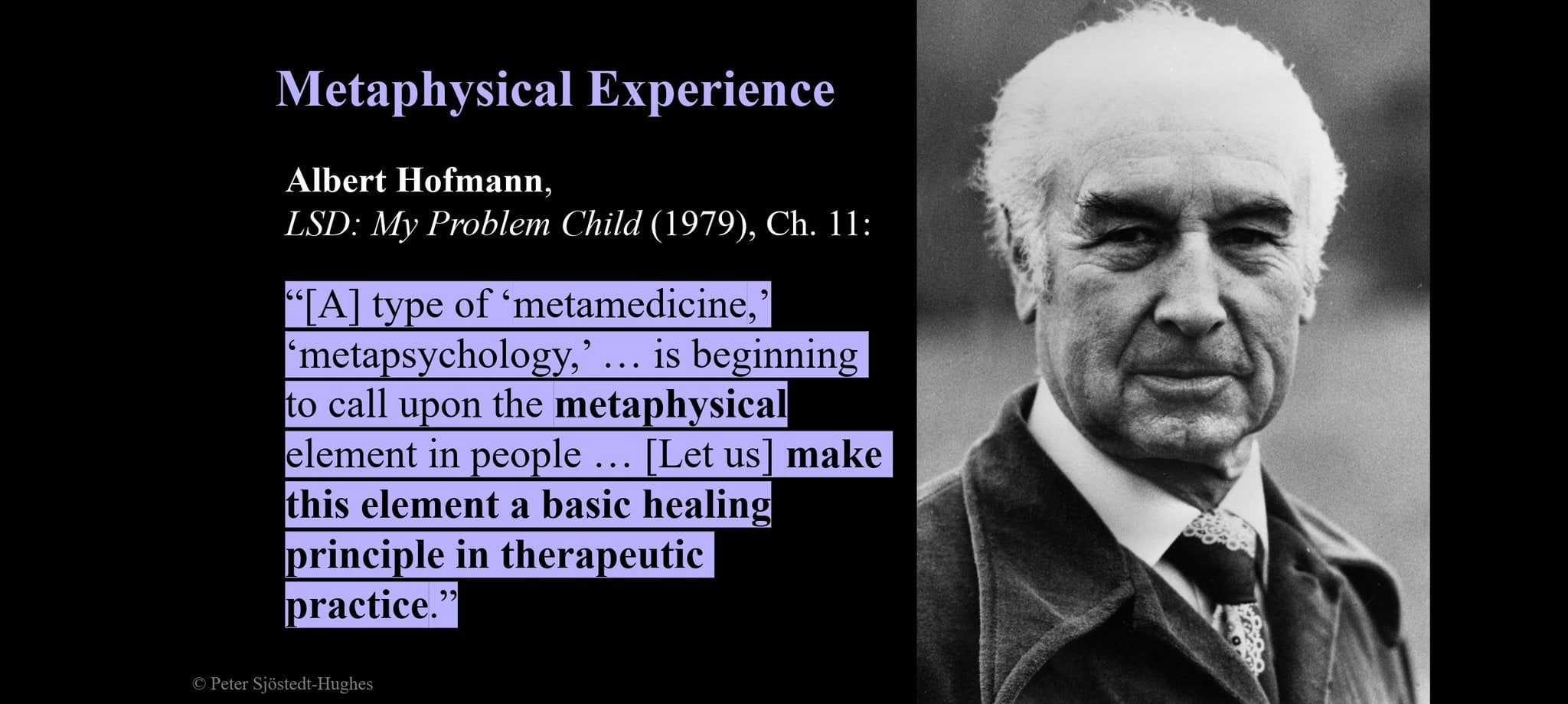
Working with leading drug discovery, Evotec, Awakn has harnessed Artificial Intelligence (AI) to discover over 100 compounds that have the ability to interact at a neurobiological level in the same way as MDMA.
It recently announced the success of its new chemical entity (NCE) development programme, which has now identified a novel MDMA-like series. Four leading compounds have been selected to be taken into in vivo analysis to assess their efficacy for substance and behavioural addictions.
“MDMA is a bit of a challenge because it takes six hours to work, with a six-hour recovery window. The NHS does not have the facility to have someone sitting in a treatment room for six hours for 12 hours, so, we are looking to develop the next generation of entactogens that will disrupt brain circuits in the way that we want them disrupted – but will work in a potentially shorter window.
“We believe, based upon the evidence available, that psychedelics have the ability to transform how mental health and addiction are treated on an international level. So, we would hope that we will be able to treat addiction with a higher level of higher efficacy. We are in a position to really have a positive impact on families, individuals and communities, who are adversely affected by addiction and mental health – we like to think we have the ability to provide hope for people for whom the current status quo is not working.
“The only way that you can monetise this is you get it through trials and marketing authorisation, so the insurance companies will reimburse the public healthcare systems, and will be able to refer patients. If we can do that collectively and collaboratively we are in a position to really provide help to an awful lot of people.
“If that doesn’t happen – if regulation doesn’t move at speed and politicians get in the way and this remains off label, and remains only available to people who can pay for these kinds of services – that is a challenge. We are fully committed to doing the right thing, which is driving the research in order to secure democratisation, but working hand in hand with the capital markets – because capital markets gives us access to the capital to enable us to move faster. That, ultimately, will enable us to help more people much faster.”
[activecampaign form=52]

 Opinion2 years ago
Opinion2 years ago
 Insight3 years ago
Insight3 years ago
 Medicinal2 years ago
Medicinal2 years ago
 Research2 years ago
Research2 years ago
 Markets & Industry1 year ago
Markets & Industry1 year ago
 Medicinal2 years ago
Medicinal2 years ago
 News3 years ago
News3 years ago
 Research2 years ago
Research2 years ago